Pain Management
-

What is Neck Pain?
Neck pain is a common symptom that you have various problems in your neck region. There are different causes of…
Read More » -

What is Shoulder Pain
Shoulder pain Shoulder pain is very common and can have different causes and treatments. There are different symptoms and causes…
Read More » -
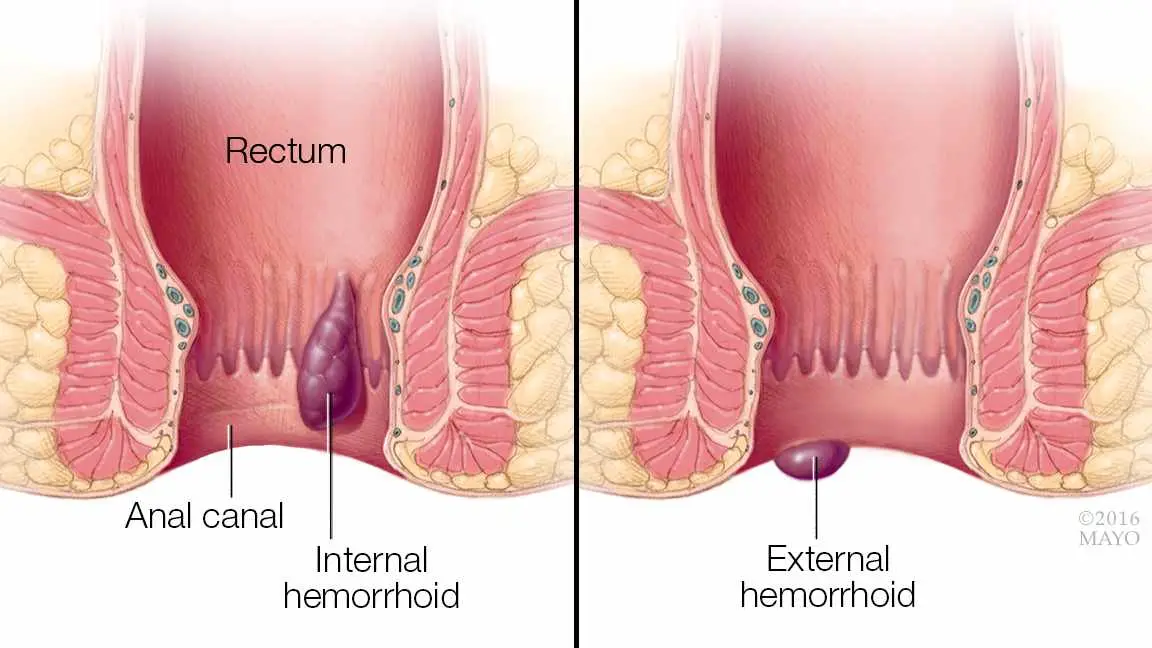
Hemorrhoid Pain Relief
Hemorrhoid is a very common condition nowadays because people’s lifestyle and eating habits are not up to the mark which…
Read More » -
Broken Tooth Pain Relief
A broken tooth can cause a lot of pain in the inner layer of your jaw and the upper side.…
Read More » -

Hemorrhoid Pain Relief
Dealing with hemorrhoid pain? You're not alone—millions suffer in silence from this common yet uncomfortable condition. This comprehensive guide reveals…
Read More » -

All Natural Tooth Pain Relief Home Remedies
When a toothache strikes at 2 AM and you're miles away from the nearest dentist, you need relief—and you need…
Read More »

