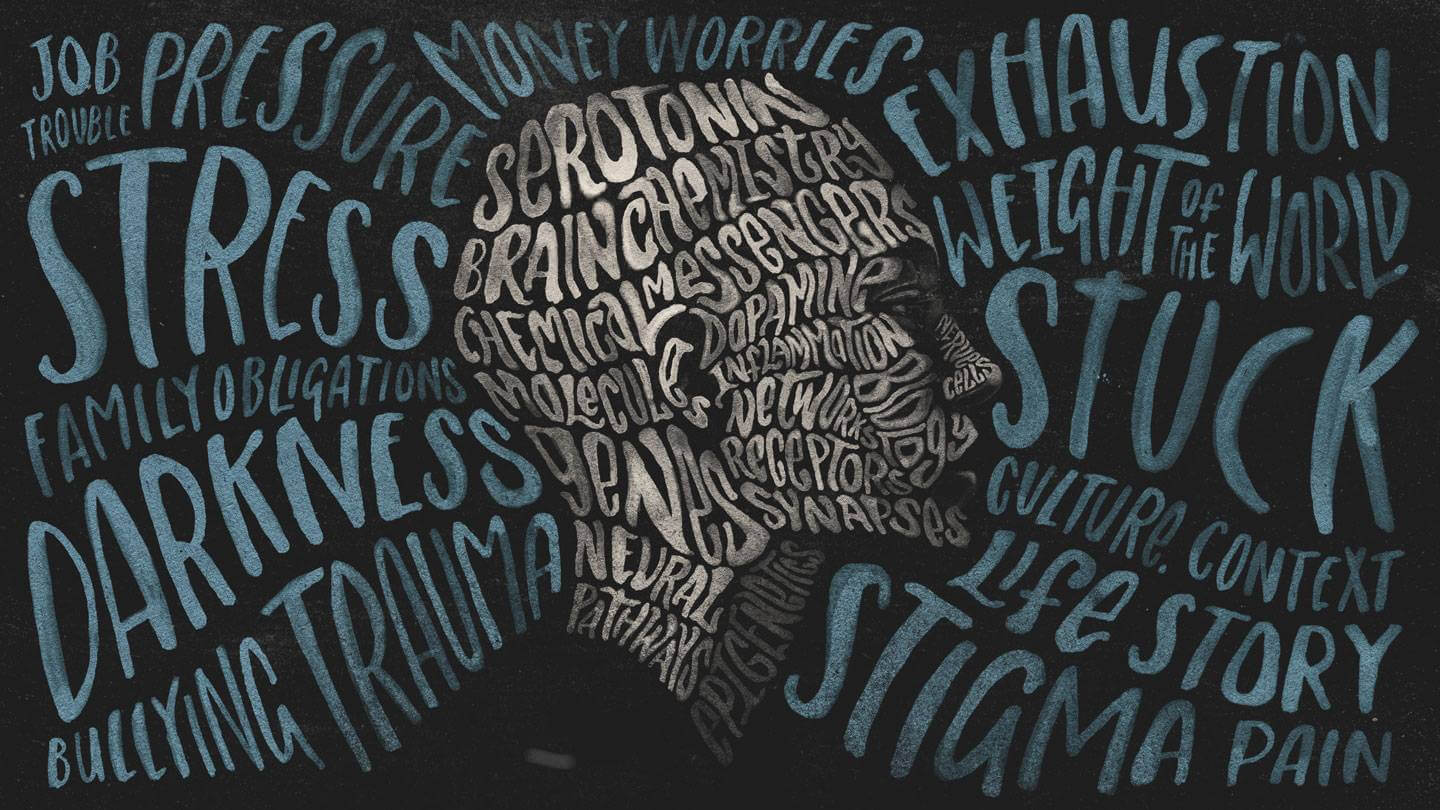
Depression and pain have a lot in common. Pain can cause depression, while depression can cause pain. Sometimes the connection between pain and depression can get out of hand, with the former exacerbating the symptoms of the latter.
Inexplicable bodily symptoms like headaches or back pain are frequently brought on by depression.
This kind of pain may be the sole or earliest sign of depression. Chronic pain can cause a variety of problems, including stress and sleep disruptions, which can lead to sadness. Low self-esteem may be brought on by problems with work or money, an incapacity to participate in social or leisure activities, or the presence of incapacitating pain.
Depression can develop for reasons other than accident-related pain. those experiencing agony because of an It is typically experienced by people with medical conditions including diabetes, cancer, or heart disease.
You might require different treatments for depression and pain to manage their respective symptoms. However, some therapies might be beneficial for both:
Antidepressant medications:
Because chemical messengers in the brain that cause both pain and depression can be relieved.
Talk therapy:
These problems can be successfully treated with psychotherapy, commonly known as psychological counseling.
Stress-reduction techniques:
Exercise, physical activity, writing, learning coping mechanisms, and other methods may also be beneficial.
Pain rehabilitation programs:
A multidisciplinary approach to treatment, including medical and behavioral components, is often provided by facilities like the comprehensive Pain Rehabilitation Centre at Mayo Clinic.
The most successful form of treatment for depression and co-occurring pain may entail a combination of therapies. Get help if you’re depressed and in pain before your symptoms get worse. You don’t need to be unhappy. The correct medical care can enable you to resume enjoying life.
Are depression and low back pain related?
Two of the most frequent causes of visits to the doctor are depression and low back pain. Despite this, the medical community has not placed much attention on the connection between these two illnesses. In this post, we’d like to highlight some fundamental details about how these related ailments might affect your health and the most effective ways to cure them so that you can get better.
For someone experiencing both melancholy and low back pain, it might be challenging to determine which disease originated from the other.
What contributes to depression the most frequently?
Depression can have a variety of reasons. The inability to engage in a favorite sport, such as golf, tennis, cycling, hiking, or even just working out, maybe the cause of the person’s depression.
Dr. William Nelson, of Explore Health in Scottsdale, Arizona, is a specialist in determining and treating the underlying causes of depression, including hormonal imbalances (for both men and women), adrenal and/or thyroid disorders, neurotransmitter deficiencies, past physical or emotional trauma, alcohol use disorders, and opiate addiction. He appreciates the value of treating both mental and physical suffering, and he has had remarkable success applying the ideas of mind-body medicine.
Patients with lower back pain frequently experience anxiety and depression.
Many persons with low back pain that also experience emotional suffering visit our center. It can be very challenging for someone who experiences back pain, anxiety, or depression to explain or communicate how severe their symptoms are to a family member, a friend, or even a medical expert. In its most basic form, resolving the back pain should subsequently resolve the issues resulting from emotional discomfort. But it’s not quite that easy. Despite the disagreements, evidence suggests that back pain, anxiety, and depression problems are more complex than just back pain issues. It is a physical issue affecting the entire body. Consequently, the question of appropriate therapies arises for a few. Some people may benefit from anti-inflammatory medicines.
What is the relationship between low back pain and depression?
Low back pain chances rise with depression:
According to studies, depression dramatically raises the chance of both sustaining an acute back injury and developing persistent low back pain.
Low back pain is more common among persons with depression:
According to statistics, two-thirds of those seeking therapy for low back pain also experience despair. persons with depression are also four times more likely to experience low back pain.
Low back pain is made worse by depression:
There is a direct correlation between a person’s low back pain and the degree of their depression.
Depression makes people more disabled by low back pain:
Additionally, it was discovered that persistent back pain and depression together were linked to more disability than either condition alone.
Combination therapy is most effective:
It’s crucial to treat individuals’ low back pain and depression concurrently. The clinical therapy of depression is hampered by chronic pain, and combined treatment is more effective than either intervention used alone.
Depression hinders postoperative recovery:
In comparison to people without depression, low back patients with depression experienced greater problems and had lower surgical results.
What are some significant depression statistics?
- Depression is a prevalent mental illness. Worldwide, depression affects more than 264 million individuals of all ages.
- Depression affects more women than males.
- Suicide can result from depression.
- Even though there are powerful psychological and pharmaceutical treatments for moderate and severe depression, up to 80% of depressed individuals never receive treatment, have a false diagnosis, or receive ineffective treatment World Health Organization Facts about Depression
Depression Psychological Theories
Control is a key component of some psychological theories on how depression manifests in people with chronic back pain. As was previously mentioned, having chronic back pain can make it more difficult to carry out several activities, including working, engaging in leisure activities, and interacting with loved ones and friends. The result of this circumstance is what has been referred to as “physical and mental reconditioning” (See Gaeltacht and Turk, 1999). The individual with chronic back pain feels a growing sense of loss of control over his or her life as the spiral continues. In the end, the person feels as though the pain has complete power over them, which causes severe depression. Once sad, a person is typically powerless to change.
Leave a Reply