Psoriasis vs Eczema: Functional Medicine Treatment
Let's face it – dealing with chronic skin conditions like psoriasis and eczema can be absolutely maddening! You've probably tried countless creams, medications, and treatments, only to find temporary relief at best. Well, here's the thing: what if I told you there's a completely different approach that's been gaining serious traction among health professionals worldwide?
Functional medicine is revolutionizing how we understand and treat skin conditions. Instead of just masking symptoms with topical treatments, this approach digs deep to uncover the root causes. It's like being a detective for your own health – pretty cool, right? This comprehensive guide will walk you through the key differences between psoriasis vs eczema and explore cutting-edge functional medicine treatments that could finally give you the lasting relief you've been searching for.
Understanding Psoriasis: More Than Skin Deep
What Exactly Is Psoriasis?
Psoriasis isn't just your average skin irritation – oh no, it's way more complex than that! This autoimmune condition occurs when your immune system goes haywire, causing skin cells to multiply at breakneck speed. Normally, skin cells take about 28 days to cycle through their life span. But with psoriasis? We're talking 3-4 days. That's like your skin being stuck in fast-forward mode!
The result is those characteristic thick, scaly patches that can appear anywhere on your body. According to the National Psoriasis Foundation, “Psoriasis occurs when the immune system sends out faulty signals that speed up the growth cycle of skin cells.” These silvery-white scales aren't just cosmetic concerns – they're often accompanied by inflammation, itching, and sometimes even joint pain.
Types and Symptoms You Should Know About
Here's where things get interesting – psoriasis isn't a one-size-fits-all condition. There are actually several types:
- Plaque psoriasis (most common) – thick, red patches with silvery scales
- Guttate psoriasis – small, drop-shaped lesions
- Inverse psoriasis – smooth, red patches in skin folds
- Pustular psoriasis – white pustules surrounded by red skin
- Erythrodermic psoriasis – widespread redness and scaling
The symptoms can vary dramatically from person to person. Some folks experience mild scaling that's barely noticeable, while others deal with extensive coverage that significantly impacts their quality of life. What's particularly frustrating is the unpredictable nature – you might have clear skin for months, then BAM! A flare-up appears seemingly out of nowhere.
Eczema Decoded: The Itch That Won't Quit
The Lowdown on Eczema
Now, let's talk about eczema – or as the medical professionals call it, atopic dermatitis (AD). Unlike psoriasis, eczema is primarily driven by a compromised skin barrier function. Think of your skin as a brick wall – in healthy skin, those “bricks” fit together perfectly, keeping moisture in and irritants out. But with eczema? Those bricks have gaps, making your skin vulnerable to dryness, irritation, and inflammation.
The American Academy of Dermatology states that “Eczema is a group of conditions that cause the skin to become red, itchy, and inflamed.” What makes eczema particularly challenging is its tendency to start early – we're talking infancy and childhood – and its strong connection to allergies and asthma. It's like the skin's way of overreacting to everyday substances that wouldn't bother most people.
Recognizing Eczema's Many Faces
Here's what makes eczema tricky to pin down – it can look completely different depending on your age and the specific type you're dealing with:
Common types include:
- Atopic dermatitis – the classic childhood eczema
- Contact dermatitis – reaction to specific irritants or allergens
- Dyshidrotic eczema – tiny, itchy blisters on hands and feet
- Nummular eczema – coin-shaped patches
- Seborrheic dermatitis – affects oily areas like the scalp
The hallmark symptom? That relentless itch that seems to intensify at the worst possible moments – usually at night when you're trying to sleep! The skin typically appears red, inflamed, and may ooze or crust over when scratched. It's a vicious cycle: you itch, you scratch, the skin gets more irritated, and the itching intensifies.
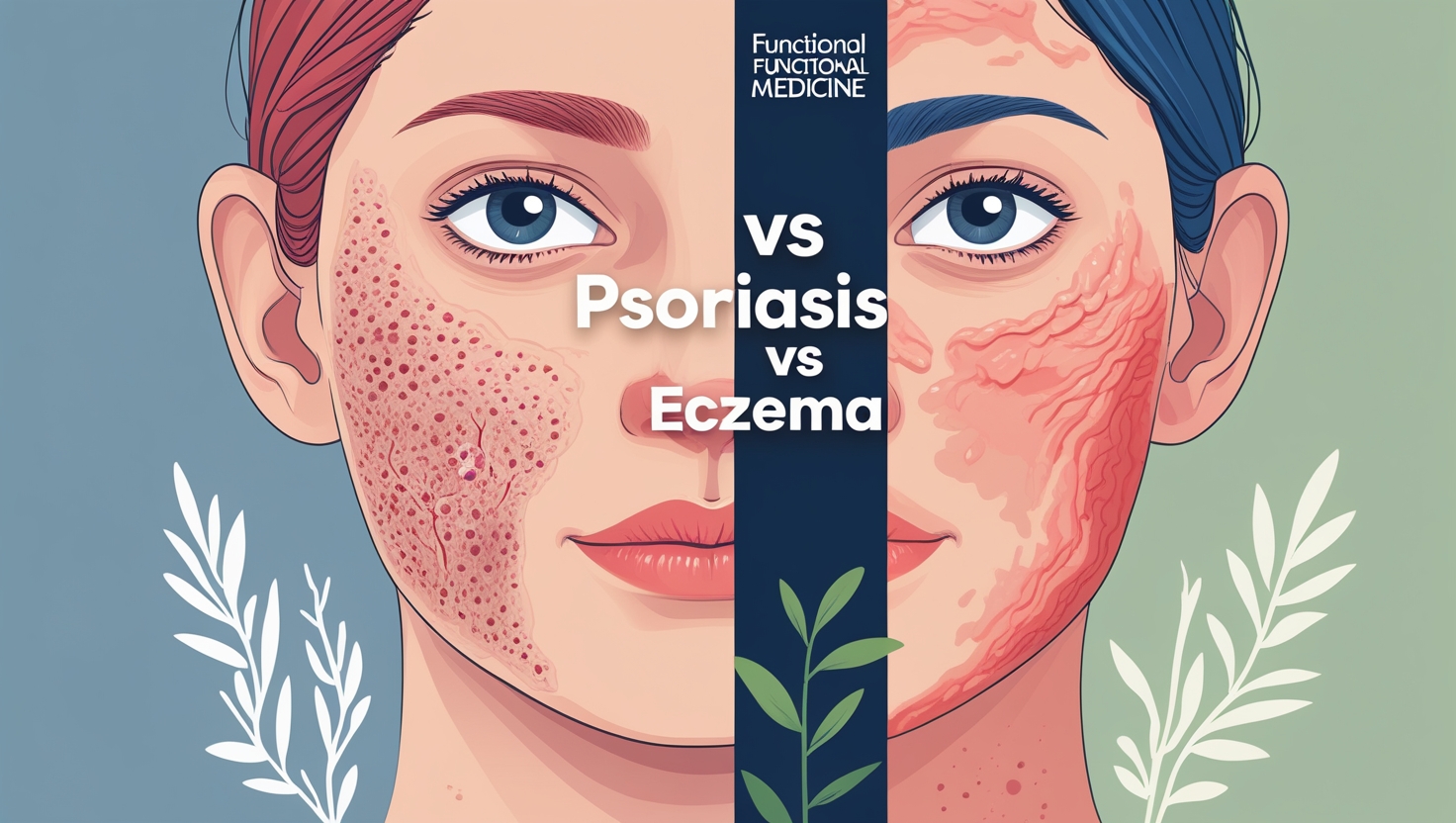
The Great Debate: Psoriasis vs Eczema Differences
Location, Location, Location
One of the most telling differences between these conditions is where they typically show up on your body. Psoriasis has its favorite spots – it loves areas where skin rubs against skin or experiences friction. We're talking elbows, knees, scalp, lower back, and around the hairline. It's like psoriasis has a preference for the “high-traffic” areas of your body!
Eczema, on the other hand, tends to be more selective about its real estate. In babies and young children, you'll often see it on the face, especially around the cheeks. As people age, it migrates to the creases – think inside the elbows, behind the knees, on the neck, and around the ankles. It's almost as if eczema prefers the more delicate, folded areas of skin.
The Look and Feel Factor
When it comes to appearance, these conditions couldn't be more different if they tried! Psoriasis patches are typically well-defined with clear borders – they look like someone drew around them with a marker. The scales are usually thick and silvery-white, and when you remove them (though you shouldn't!), you might see tiny bleeding points underneath.
Eczema presents a completely different picture. The affected areas tend to be more diffuse with poorly defined borders that seem to blend into normal skin. The texture is usually rough and bumpy rather than scaly, and the color can range from red to brown, depending on your skin tone. Plus, eczema often shows signs of scratching – think lichenification (thickened skin from chronic scratching) and sometimes open sores from excessive itching.
Root Causes: What's Really Going On?
The Psoriasis Puzzle
Understanding what triggers psoriasis is like solving a complex puzzle with multiple pieces. At its core, it's an autoimmune condition where T-cells (your immune system's soldiers) mistakenly attack healthy skin cells. But what sets this whole process in motion? Well, that's where it gets interesting!
Research published in the Journal of Clinical Medicine suggests that psoriasis involves a complex interplay of genetic predisposition, environmental triggers, and immune system dysfunction. Common triggers include stress (both physical and emotional), infections (particularly strep throat), certain medications, skin injuries, and even weather changes. Some folks notice flare-ups during winter months when humidity drops and skin becomes drier.
But here's where functional medicine gets really fascinating – practitioners look beyond these surface triggers to examine deeper imbalances. They consider factors like gut health, food sensitivities, nutrient deficiencies, hormonal imbalances, and chronic inflammation throughout the body. It's a holistic approach that recognizes your skin as a reflection of your overall health status.
Unraveling Eczema's Mysteries
Eczema's story is quite different, though equally complex. At its foundation lies a defective skin barrier – specifically, problems with a protein called filaggrin that helps maintain the skin's protective function. When this barrier is compromised, your skin loses moisture more rapidly and becomes more susceptible to irritants, allergens, and bacterial infections.
The National Eczema Association explains that eczema often involves what's called the “atopic march” – a progression from eczema in infancy to food allergies, asthma, and environmental allergies later in life. This connection highlights how eczema isn't just a skin problem but part of a broader pattern of immune system hypersensitivity.
Environmental factors play a huge role too. Common triggers include harsh soaps and detergents, synthetic fabrics, extreme temperatures, stress, hormonal fluctuations, and exposure to allergens like dust mites, pet dander, or certain foods. It's like your skin has become hypersensitive to the world around it!
Functional Medicine: A Game-Changing Approach
Why Functional Medicine Makes Sense
Here's where things get really exciting! Traditional dermatology, while valuable, often focuses on symptom management through topical treatments and immunosuppressive medications. Don't get me wrong – these approaches definitely have their place and can provide much-needed relief. But functional medicine asks a different question entirely: “Why is this happening in the first place?”
This approach recognizes that skin conditions are rarely just about the skin. Your dermatological health is intimately connected to your digestive system, immune function, hormonal balance, stress levels, and overall nutritional status. According to the Institute for Functional Medicine, this systems-based approach “addresses the underlying causes of disease, using a systems-oriented approach and engaging both patient and practitioner in a therapeutic partnership.”
What makes functional medicine particularly powerful for psoriasis vs eczema treatment is its personalized nature. Instead of applying a one-size-fits-all approach, practitioners conduct comprehensive assessments to understand your unique biochemistry, genetic predispositions, lifestyle factors, and environmental exposures. It's like having a custom-tailored treatment plan designed specifically for your body's needs.
The Functional Medicine Toolkit
Functional medicine practitioners have an impressive arsenal of assessment tools and treatment modalities at their disposal. They might start with detailed questionnaires about your health history, lifestyle, stress levels, and dietary patterns. But they don't stop there – oh no, they dig deeper!
Advanced laboratory testing often includes comprehensive stool analyses to assess gut microbiome diversity and intestinal permeability (aka “leaky gut”). They might check for food sensitivities, environmental toxin exposure, nutrient deficiencies, hormonal imbalances, and inflammatory markers throughout your body. Some practitioners even utilize genetic testing to understand how your body processes certain nutrients or detoxifies harmful substances.
The treatment protocols are equally comprehensive and might include targeted nutritional interventions, specific supplements, stress management techniques, sleep optimization strategies, exercise recommendations, and environmental toxin reduction. It's a multi-pronged approach that addresses all the potential contributing factors simultaneously.
Gut-Skin Connection: The Missing Link
Your Second Brain and Your Skin
Prepare to have your mind blown – did you know that your gut and skin are in constant communication? Scientists have discovered what's called the “gut-skin axis,” a bidirectional communication pathway between your digestive system and your skin. This connection is so profound that many functional medicine practitioners consider gut health the foundation of healthy skin.
Research published in Clinical Reviews in Allergy & Immunology demonstrates that the gut microbiome significantly influences skin inflammation and immune responses. When your gut microbiome is imbalanced (a condition called dysbiosis), it can trigger systemic inflammation that manifests as skin problems. It's like having an internal fire that shows up as external symptoms!
The mechanism involves several pathways. An imbalanced gut can increase intestinal permeability, allowing harmful substances to enter your bloodstream and trigger immune responses. This chronic low-grade inflammation can exacerbate both psoriasis and eczema. Additionally, certain beneficial bacteria in your gut produce short-chain fatty acids and other compounds that help regulate immune function and reduce inflammation throughout your body.
Healing from the Inside Out
So how do functional medicine practitioners address this gut-skin connection? The approach typically starts with comprehensive gut restoration protocols. This might involve eliminating inflammatory foods, introducing gut-healing nutrients, and repopulating the microbiome with beneficial bacteria through targeted probiotics and prebiotic-rich foods.
Common interventions include:
- Elimination diets to identify food triggers
- Anti-inflammatory protocols featuring omega-3 fatty acids and polyphenol-rich foods
- Gut barrier support with nutrients like L-glutamine, zinc, and vitamin D
- Microbiome restoration through diverse probiotic strains and fermented foods
- Digestive enzyme support to optimize nutrient absorption
The timeline for seeing improvements can vary dramatically – some people notice changes within weeks, while others might need several months of consistent intervention. But here's the beautiful thing: when you heal your gut, you often see improvements that go far beyond your skin. We're talking better energy, improved mood, enhanced immune function, and overall better health!
Anti-Inflammatory Nutrition Strategies
Foods That Fight Fire
When it comes to managing psoriasis vs eczema through nutrition, think of food as either fuel for the fire or water to put it out. Chronic inflammation is at the root of both conditions, so adopting an anti-inflammatory eating pattern can be incredibly powerful for symptom management and overall health improvement.
The Mediterranean diet has shown particular promise for inflammatory skin conditions. This eating pattern emphasizes omega-3 rich fish, colorful vegetables and fruits, nuts, seeds, olive oil, and herbs with potent anti-inflammatory compounds. Research published in Nutrients suggests that adherence to Mediterranean dietary patterns is associated with reduced inflammatory markers and improved skin health outcomes.
Key anti-inflammatory foods to emphasize include fatty fish like salmon and sardines (rich in omega-3s), leafy greens packed with antioxidants, colorful berries loaded with polyphenols, nuts and seeds providing healthy fats and minerals, and spices like turmeric and ginger with powerful anti-inflammatory compounds. It's like building an internal pharmacy with every meal!
What to Avoid (And Why)
Just as important as what you include is what you eliminate or reduce. Certain foods can act as inflammatory triggers, potentially worsening symptoms in susceptible individuals. Common culprits include highly processed foods loaded with preservatives and artificial additives, refined sugars that promote inflammatory pathways, trans fats found in fried and packaged foods, and excessive omega-6 oils that can shift your inflammatory balance.
For some people, specific food sensitivities play a major role in symptom flares. Common triggers include:
- Gluten – may increase intestinal permeability in sensitive individuals
- Dairy products – can be inflammatory for those with lactose intolerance or casein sensitivity
- Nightshade vegetables (tomatoes, peppers, eggplant) – contain alkaloids that some people react to
- High-histamine foods – particularly problematic for those with histamine intolerance
- Alcohol – can disrupt gut barrier function and increase inflammation
The key is identifying your individual triggers through systematic elimination and reintroduction protocols, often guided by functional medicine practitioners who can provide personalized guidance and support throughout the process.
Supplement Strategies That Work
The Power Players
While food should always be your foundation, targeted supplementation can provide additional support for healing and symptom management. Functional medicine practitioners often recommend specific nutrients based on individual testing and clinical presentation, but several supplements have shown particular promise for both psoriasis and eczema.
Omega-3 fatty acids top the list for their potent anti-inflammatory effects. High-quality fish oil supplements providing EPA and DHA can help balance inflammatory pathways and support skin barrier function. The American Journal of Clinical Dermatology has published studies showing significant improvements in psoriasis severity with omega-3 supplementation.
Vitamin D deserves special mention – many people with inflammatory skin conditions have suboptimal vitamin D levels, and this nutrient plays crucial roles in immune regulation and skin cell development. Probiotics are another game-changer, particularly multi-strain formulations that support gut microbiome diversity and reduce systemic inflammation.
Targeted Nutritional Support
Beyond the basics, several nutrients have shown specific benefits for skin health and inflammation management:
For barrier function support:
- Zinc – essential for wound healing and immune function
- Vitamin A – crucial for skin cell differentiation and repair
- Essential fatty acids – support cell membrane integrity
- Vitamin E – provides antioxidant protection
For inflammation management:
- Curcumin – powerful anti-inflammatory compound from turmeric
- Quercetin – natural antihistamine and anti-inflammatory
- N-acetylcysteine (NAC) – supports detoxification and reduces oxidative stress
- Alpha-lipoic acid – versatile antioxidant that regenerates other antioxidants
The dosing and timing of these supplements should always be individualized based on your specific needs, current health status, and any medications you might be taking. This is where working with a knowledgeable functional medicine practitioner becomes invaluable – they can design a targeted protocol that's both safe and effective for your unique situation.
Stress Management and Mind-Body Medicine
The Stress-Skin Spiral
Let's talk about something that's often overlooked in conventional treatment approaches – the profound connection between your mental/emotional state and your skin health. Stress isn't just something that makes you feel frazzled; it's a powerful trigger for both psoriasis and eczema flares. And here's the kicker – having a visible skin condition can create additional stress, leading to a vicious cycle that's hard to break!
When you're stressed, your body releases cortisol and other stress hormones that can disrupt immune function, increase inflammation, and compromise your skin's barrier function. According to research published in Dermatology Online Journal, psychological stress can directly trigger inflammatory cascades in the skin and worsen existing conditions.
But it's not just acute stress we need to worry about – chronic, low-grade stress from work pressures, relationship issues, financial concerns, or health worries can keep your body in a constant state of inflammatory alert. It's like having your internal alarm system stuck in the “on” position, which takes a tremendous toll on your overall health and skin specifically.
Proven Stress-Busting Strategies
The good news? There are numerous evidence-based techniques for managing stress and supporting your skin health from the inside out. Mind-body practices have shown particular promise for people dealing with inflammatory skin conditions.
Effective stress management approaches include:
- Meditation and mindfulness – regular practice can reduce cortisol levels and inflammatory markers
- Deep breathing exercises – activate the parasympathetic nervous system and promote relaxation
- Progressive muscle relaxation – helps release physical tension and mental stress
- Yoga and tai chi – combine movement, breath work, and mindfulness for comprehensive benefits
- Regular exercise – natural stress reliever that also supports immune function
- Adequate sleep – crucial for stress recovery and skin repair processes
Many functional medicine practitioners also incorporate techniques like biofeedback, cognitive-behavioral therapy (CBT), and even clinical hypnosis for stress management. The key is finding approaches that resonate with you and can be consistently maintained as part of your daily routine.
Detoxification and Environmental Factors
Your Toxic Load Matters
Here's something that might surprise you – your skin is your body's largest organ of elimination! When your other detoxification pathways (liver, kidneys, lungs) become overwhelmed, your skin often picks up the slack. This is why environmental toxin exposure can play a significant role in inflammatory skin conditions like psoriasis and eczema.
We're exposed to thousands of chemicals daily through our food, water, air, personal care products, and household cleaners. While our bodies are designed to handle reasonable toxin loads, the modern environment can overwhelm our natural detoxification systems. Research in Environmental Health Perspectives has linked various environmental exposures to increased inflammatory skin conditions.
Common environmental triggers include heavy metals (lead, mercury, cadmium), volatile organic compounds (VOCs) from cleaning products and new furniture, pesticides and herbicides from non-organic foods, phthalates and parabens from personal care products, and air pollution from vehicle exhaust and industrial emissions. It's like your skin is trying to deal with a constant barrage of foreign substances!
Creating a Cleaner Environment
The good news is that you have more control over your toxic exposure than you might think! Functional medicine practitioners often recommend a systematic approach to reducing environmental triggers and supporting your body's natural detoxification processes.
Practical detox strategies include:
- Clean up your personal care routine – choose products with minimal, recognizable ingredients
- Improve indoor air quality – use HEPA filters and increase ventilation
- Filter your water – remove chlorine, fluoride, and other contaminants
- Choose organic foods when possible, especially for the “dirty dozen” produce items
- Use natural cleaning products – or make your own with simple ingredients like vinegar and baking soda
- Support detox pathways through adequate hydration, fiber intake, and regular exercise
- Consider targeted detox support – such as infrared saunas, dry brushing, or specific supplements
Remember, detoxification isn't about extreme cleanses or fasting protocols – it's about reducing your daily toxic load while supporting your body's natural ability to eliminate harmful substances. Small, consistent changes often yield the most sustainable results!
Success Stories and Real-World Results
When Everything Clicks
I wish you could meet Sarah, a 34-year-old marketing executive who'd been battling severe psoriasis for over a decade. She'd tried every topical treatment, several systemic medications, and even light therapy with only temporary improvements. When she first walked into her functional medicine practitioner's office, she was frustrated, exhausted, and honestly pretty skeptical about yet another approach.
Her comprehensive assessment revealed several key findings: significant gut dysbiosis, multiple food sensitivities (including gluten and dairy), vitamin D deficiency, chronic stress from her high-pressure job, and elevated inflammatory markers. Her practitioner designed a multi-faceted protocol addressing each of these areas systematically.
Within three months of implementing dietary changes, targeted supplementation, stress management techniques, and gut healing protocols, Sarah noticed her psoriasis plaques beginning to shrink and become less inflamed. By the six-month mark, her skin was 80% clear – something she hadn't experienced in years! But perhaps more importantly, she reported better energy, improved mood, better sleep, and an overall sense of vitality she'd forgotten was possible.
The Eczema Breakthrough
Then there's Michael, a 28-year-old teacher whose severe eczema had plagued him since childhood. The constant itching was affecting his sleep, his job performance, and his self-confidence. Traditional treatments provided temporary relief but never addressed the underlying issues driving his condition.
His functional medicine evaluation uncovered a fascinating connection – his eczema flares consistently coincided with high-stress periods at work and seemed to worsen with certain environmental exposures in his classroom. Testing revealed poor detoxification capacity, low levels of anti-inflammatory nutrients, and an imbalanced gut microbiome likely stemming from years of antibiotic use for recurring infections.
His personalized protocol focused on supporting detoxification pathways, healing his gut microbiome, addressing nutrient deficiencies, and implementing practical stress management strategies he could use even during busy school days. The transformation wasn't immediate – it took about four months to see significant improvement – but the results were remarkable. His eczema didn't just improve; it virtually disappeared, and he felt better overall than he had in decades.
Frequently Asked Questions
Q: How long does it take to see results with functional medicine approaches? A: The timeline varies significantly based on individual factors, but most people begin noticing improvements within 4-8 weeks of starting a comprehensive protocol. Full resolution of symptoms typically takes 3-6 months or longer, depending on the severity of the condition and how long it's been present.
Q: Can I use functional medicine approaches alongside conventional treatments? A: Absolutely! Functional medicine is designed to complement, not replace, conventional medical care. Many people find the best results come from integrating both approaches under the guidance of qualified healthcare providers.
Q: Are functional medicine treatments covered by insurance? A: Coverage varies widely depending on your insurance plan and the specific practitioner. Some functional medicine doctors are MDs who accept insurance, while others operate on a cash-pay basis. It's worth checking with your provider and exploring options like Health Savings Accounts (HSAs) for coverage.
Q: Is it safe to stop my prescription medications when starting functional medicine? A: Never discontinue prescription medications without consulting your prescribing physician! Functional medicine practitioners typically work to support your overall health while you continue necessary medications, with the goal of potentially reducing medication dependence over time under medical supervision.
Q: How do I find a qualified functional medicine practitioner? A: Start with the Institute for Functional Medicine's practitioner directory to locate certified practitioners in your area. Look for providers with additional training in dermatology or experience treating skin conditions specifically.
Q: What's the difference between functional medicine and naturopathic medicine? A: While both approaches focus on root causes and natural healing, functional medicine is a systems-based approach that can be practiced by various types of healthcare providers (MDs, DOs, NDs, etc.), while naturopathic medicine is a distinct medical profession with its own training and philosophy.
Final Thoughts: Your Journey to Healthier Skin
As we wrap up this comprehensive exploration of psoriasis vs eczema and functional medicine treatments, I hope you're feeling inspired and empowered about the possibilities ahead. The journey to healthier skin isn't always linear – there might be setbacks, adjustments to your protocol, and times when progress feels frustratingly slow. But remember, you're not just treating symptoms; you're addressing the root causes and building a foundation for long-term health and vitality.
The functional medicine approach to psoriasis vs eczema represents a paradigm shift in how we think about skin health. Instead of viewing these conditions as isolated problems requiring symptom suppression, we're recognizing them as manifestations of deeper imbalances that, when addressed comprehensively, can lead to profound healing and transformation.
Whether you're just beginning to explore functional medicine approaches or you're already on your healing journey, remember that every small step matters. The dietary changes you make today, the stress management techniques you practice, the environmental toxins you eliminate – they all contribute to your body's incredible capacity for healing and regeneration.
Your skin has an amazing ability to heal when given the right support and conditions. By addressing the root causes through comprehensive functional medicine approaches, you're not just working toward clearer skin – you're investing in your overall health, vitality, and quality of life for years to come. Here's to your journey toward healthier skin and a healthier you!