Understanding Sciatica: A Major Cause of Lower Back Pain
Sciatica affects millions worldwide, causing excruciating pain that radiates from the lower back down through the legs. This comprehensive guide explores the anatomy, causes, symptoms, and treatment options for this debilitating condition that impacts daily life for so many sufferers.
What Exactly Is Sciatica?
Let's cut to the chase – sciatica isn't just your run-of-the-mill backache. Nope, it's a specific type of nerve pain that'll knock you off your feet faster than you can say “ouch!” The term “sciatica” refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg.
Here's the kicker: sciatica typically affects only one side of your body. The sciatic nerve is actually the longest and widest nerve in the human body – we're talking about a nerve that's as thick as your thumb! When this bad boy gets irritated or compressed, well, that's when the real trouble begins. According to the American Academy of Orthopaedic Surgeons, approximately 40% of people will experience sciatica at some point in their lives.
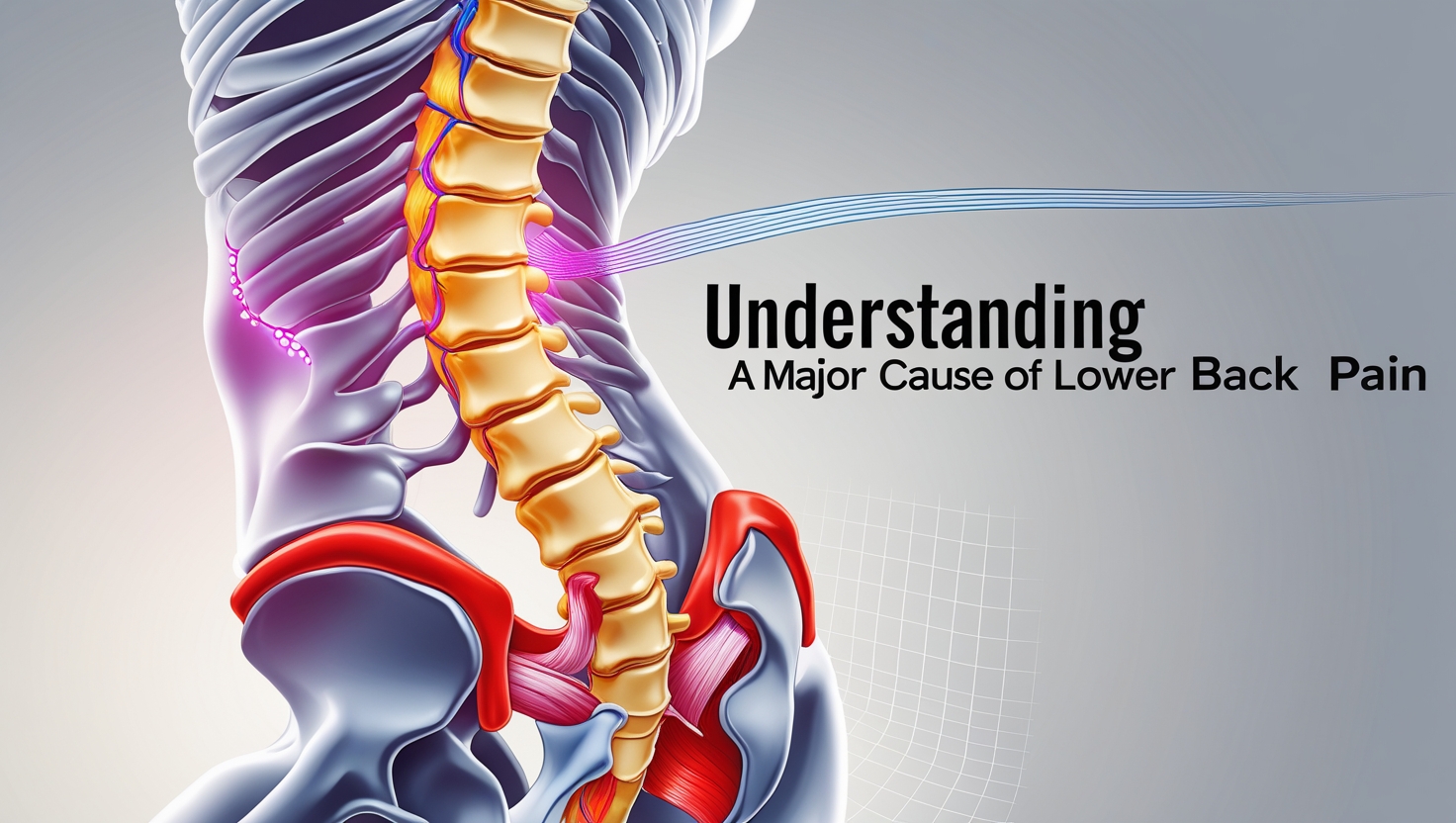
The Anatomy Behind the Agony
Understanding sciatica means getting up close and personal with your body's wiring system. The sciatic nerve originates from nerve roots in the lumbar spine (that's your lower back, folks) – specifically from the L4, L5, S1, S2, and S3 nerve roots. These nerve roots come together like tributaries forming a river, creating the massive sciatic nerve.
But wait, there's more! This nerve doesn't just hang out in your back doing nothing. Oh no, it's got places to go and muscles to innervate. The sciatic nerve travels through the piriformis muscle (remember this troublemaker), down the back of each leg, and eventually branches out to provide sensation and motor function to your lower leg and foot. When something goes awry anywhere along this pathway – boom! – you've got yourself a case of sciatica that'll make you rethink every movement.
Common Culprits: What Causes Sciatica?
Herniated Discs: The Usual Suspects
Let's talk about the most common villain in the sciatica story – herniated discs. These gel-filled cushions between your vertebrae can bulge or rupture, pressing against the nerve roots that form the sciatic nerve. Think of it like a jelly donut that's been squeezed too hard – the filling oozes out and creates a mess.
Research published in the Journal of Neurosurgery shows that disc herniation accounts for approximately 90% of sciatica cases in patients under 50. The L4-L5 and L5-S1 disc levels are particularly prone to herniation because they bear the brunt of your body weight and movement stress. Yikes!
Spinal Stenosis: When Space Gets Tight
Spinal stenosis occurs when the spinal canal narrows, squeezing the nerves like a too-tight pair of jeans after Thanksgiving dinner. This condition is more common in folks over 60, as wear and tear takes its toll on the spine. The narrowing can happen due to bone spurs, thickened ligaments, or simply the natural aging process.
What's particularly frustrating about spinal stenosis is that symptoms often worsen with walking or standing and improve when sitting or leaning forward. It's like your spine is telling you, “Hey, slow down there, speed racer!”
Piriformis Syndrome: The Sneaky Troublemaker
Here's where things get interesting – and by interesting, I mean incredibly annoying. Piriformis syndrome occurs when the piriformis muscle (a small muscle deep in your buttock) spasms or becomes tight, irritating the sciatic nerve that runs nearby or sometimes right through it. Talk about being in the wrong place at the wrong time!
This condition is often misdiagnosed because its symptoms mimic other causes of sciatica. Athletes and people who sit for long periods are particularly susceptible. The American Physical Therapy Association notes that piriformis syndrome accounts for about 6-8% of sciatica cases.
Recognizing the Red Flags: Sciatica Symptoms
The Pain That Changes Everything
Sciatica pain isn't your garden-variety discomfort – it's a game-changer that can transform your daily routine into an obstacle course. The pain typically starts in the lower back or buttock and radiates down the back of your thigh and leg. Some describe it as a sharp, shooting pain, while others experience a burning sensation or electric shock-like jolts.
But here's the thing – sciatica doesn't always play by the rules. Sometimes the pain is constant, other times it's intermittent. It might worsen when you cough, sneeze, or sit for extended periods. Standing up from a seated position? That can be pure torture. The intensity can range from mild discomfort to debilitating pain that makes you question your life choices.
Beyond Pain: The Other Players
Pain might be the star of the show, but it's got a supporting cast that includes:
- Numbness and tingling: That pins-and-needles sensation that makes your leg feel like it's “asleep”
- Muscle weakness: Difficulty lifting your foot or pointing your toes
- Loss of reflexes: Your knee-jerk reflex might go MIA
- Burning sensations: Like someone's holding a hot iron to your leg
These symptoms can occur anywhere along the sciatic nerve pathway, from your lower back all the way down to your toes. The location and type of symptoms often provide clues about where the nerve compression is occurring.
Getting to the Bottom of It: Diagnosis
The Clinical Detective Work
Diagnosing sciatica is like being a detective – you need to gather clues and piece together the puzzle. Healthcare providers start with a thorough medical history and physical examination. They'll ask about your pain patterns, what makes it better or worse, and how it affects your daily activities.
The physical exam includes several tests that might make you feel like you're auditioning for Cirque du Soleil. The straight leg raise test is a classic – you lie on your back while the provider lifts your leg. If this reproduces your pain, it's a strong indicator of sciatica. Other tests check your reflexes, muscle strength, and sensation.
High-Tech Helpers: Imaging Studies
Sometimes clinical evaluation isn't enough, and that's when technology steps in. MRI (Magnetic Resonance Imaging) is the gold standard for visualizing soft tissues like discs, nerves, and muscles. It can show disc herniations, spinal stenosis, and other structural abnormalities with remarkable detail.
CT scans might be used when MRI isn't available or suitable, and X-rays can rule out fractures or other bone problems. However, here's a reality check – imaging findings don't always correlate with symptoms. You might have a “terrible-looking” MRI but minimal pain, or vice versa. The human body loves to keep us guessing!
Treatment Options: Your Road to Recovery
Conservative Care: Starting Simple
The good news? Most cases of sciatica resolve with conservative treatment. We're talking about a multi-pronged approach that doesn't involve going under the knife. Physical therapy is often the cornerstone of treatment, focusing on exercises that improve flexibility, strengthen supporting muscles, and promote proper posture.
Anti-inflammatory medications like NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) can help reduce both pain and inflammation around the affected nerve. Sometimes muscle relaxants or even short courses of oral steroids are prescribed for severe cases. Heat and ice therapy, while simple, can provide significant relief when used correctly.
When Conservative Care Isn't Enough
For persistent or severe cases, more aggressive treatments might be necessary. Epidural steroid injections can deliver powerful anti-inflammatory medication directly to the affected area, providing relief that can last weeks or months. These injections are performed under X-ray guidance to ensure precision.
Physical therapy modalities like ultrasound, electrical stimulation, and manual therapy techniques can complement exercise programs. Some patients find relief with alternative treatments like acupuncture or chiropractic care, though the evidence for these approaches varies.
The Surgical Solution
Surgery is typically reserved for cases where conservative treatment has failed and symptoms are severe or progressive. The type of surgery depends on the underlying cause – discectomy for herniated discs, laminectomy for spinal stenosis, or other procedures as indicated.
According to research published in the New England Journal of Medicine, surgery can provide faster initial relief compared to conservative treatment, but long-term outcomes are often similar. The decision for surgery should never be taken lightly and requires careful consideration of risks and benefits.
Prevention: Your Best Defense
Lifestyle Modifications That Matter
Prevention, as they say, is worth a pound of cure – and when it comes to sciatica, this couldn't be more true. Maintaining a healthy weight reduces stress on your spine, while regular exercise keeps your core muscles strong and your spine flexible. But not just any exercise will do – you need the right kind of movement.
Low-impact activities like swimming, walking, and yoga are excellent choices. Strengthening exercises for your core, back, and leg muscles provide the stability your spine craves. Flexibility exercises, particularly for your hamstrings and hip flexors, can prevent the tightness that contributes to nerve compression.
Ergonomics and Daily Habits
Your daily habits can either protect your spine or set you up for trouble. Proper lifting technique – bending your knees, not your back – is crucial. When sitting for long periods, use a chair that supports your lower back's natural curve, and take frequent breaks to stand and move around.
Sleep posture matters too! A medium-firm mattress with proper pillow support can make a significant difference. If you're a side sleeper, try placing a pillow between your knees to maintain spinal alignment.
Frequently Asked Questions
Q: How long does sciatica typically last? A: Most acute sciatica episodes resolve within 4-6 weeks with proper treatment. However, chronic cases can persist for months or even years if underlying causes aren't addressed.
Q: Can sciatica cause permanent damage? A: While most sciatica cases resolve without permanent damage, severe or prolonged compression can lead to lasting nerve damage, muscle weakness, or sensory loss.
Q: Is it safe to exercise with sciatica? A: Gentle, appropriate exercises are often beneficial for sciatica. However, it's important to work with a healthcare provider or physical therapist to develop a safe exercise program.
Q: When should I see a doctor for sciatica? A: Seek immediate medical attention if you experience severe pain, progressive weakness, loss of bowel or bladder control, or if conservative measures don't provide relief within a few weeks.
Q: Can stress make sciatica worse? A: Yes, stress can increase muscle tension and inflammation, potentially worsening sciatica symptoms. Stress management techniques can be an important part of treatment.
Wrapping It Up: Your Journey Forward
Understanding sciatica empowers you to take control of your health and make informed decisions about treatment. This condition, while challenging, is manageable with the right approach and professional guidance. Remember, every person's experience with sciatica is unique – what works for your neighbor might not work for you, and that's perfectly normal.
The key is persistence and patience. Recovery from sciatica often takes time, and setbacks are part of the process. Work closely with your healthcare team, stay consistent with your treatment plan, and don't lose hope. Many people who suffer from sciatica go on to live active, pain-free lives with proper management and prevention strategies.
Whether you're dealing with your first episode of sciatica or you're a seasoned veteran of this nerve-wracking condition, knowledge is your most powerful tool. Stay informed, stay active within your limits, and remember – you're not alone in this journey.