What is Lower Back Pain
Lower back pain affects nearly 80% of adults at some point in their lives, making it one of the most prevalent health issues worldwide. But what exactly is lower back pain, and why does it seem to plague so many of us? This comprehensive guide breaks down everything you need to know about this frustrating condition.
Ouch! There it is again – that nagging ache in your lower back that seems to appear out of nowhere. You're definitely not alone in this struggle. Lower back pain, medically known as lumbago, is practically an epidemic in our modern world. Whether you're a desk jockey hunched over spreadsheets or a weekend warrior who overdid it at the gym, understanding what's happening in your lower back is the first step toward finding relief.
The lumbar region of your spine – that's the fancy term for your lower back – consists of five vertebrae (L1-L5) that bear most of your body's weight. When something goes haywire in this area, boy, do you feel it! From muscle strains to disc problems, the causes are as varied as they are frustrating.
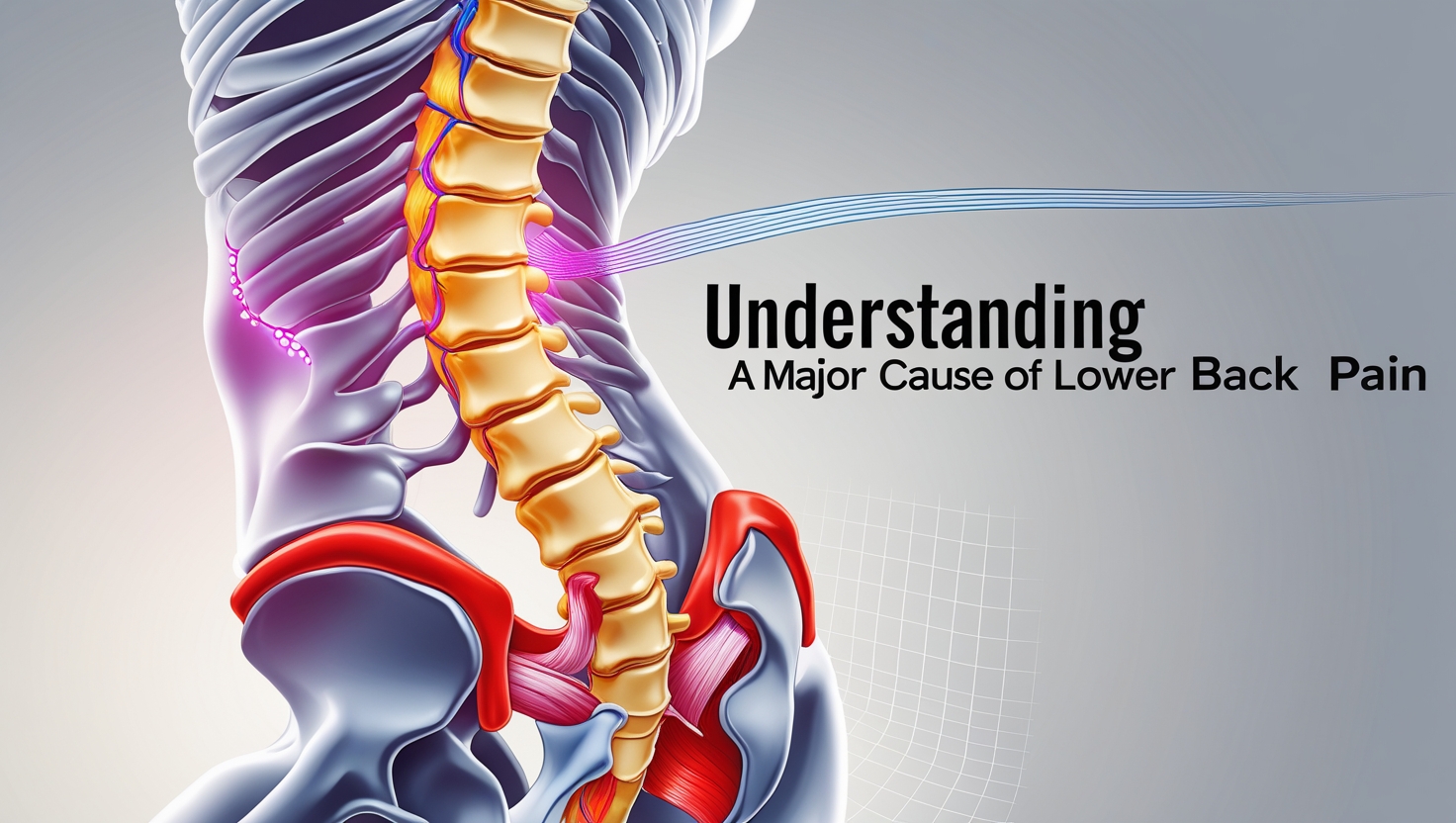
Understanding the Anatomy: What Makes Your Lower Back Tick?
Your lower back isn't just a simple structure – it's actually a complex masterpiece of engineering that would make any architect jealous. The lumbar spine consists of bones, muscles, ligaments, tendons, and those infamous discs that everyone seems to worry about. Think of it as nature's shock absorber system, designed to support your upper body while allowing you to bend, twist, and move with grace.
The vertebrae in your lower back are larger than those in your neck or upper back, and for good reason. They're literally carrying the weight of your world – or at least your torso! Between each vertebra sits a disc, which acts like a jelly-filled cushion. These discs are about 80% water when we're young, but as we age, they start to lose moisture. It's like watching a grape slowly turn into a raisin, except way less appetizing and infinitely more painful.
The Usual Suspects: Common Causes of Lower Back Pain
Mechanical Issues
Most lower back pain – we're talking about 85% of cases – falls into the mechanical category. This means there's a problem with how the parts of your back move and work together. Muscle strains are the most common culprits, often caused by lifting something too heavy, sudden movements, or maintaining poor posture for extended periods.
Herniated discs are another frequent troublemaker. Picture a jelly donut getting squeezed until the filling pops out – that's essentially what happens when a disc herniates. The “jelly” (nucleus pulposus) pushes through the outer ring (annulus fibrosus), potentially pressing on nearby nerves. Ouch!
Lifestyle Factors
Let's be honest – our modern lifestyle isn't doing our backs any favors. Prolonged sitting, especially with poor ergonomics, puts tremendous pressure on our lumbar discs. In fact, sitting increases disc pressure by up to 40% compared to standing. That's why office workers and long-distance drivers are particularly susceptible to lower back issues.
Lack of exercise creates a double whammy effect. Weak core muscles can't properly support the spine, while tight hip flexors from sitting pull on the lower back. It's like having a weak foundation trying to support a heavy structure – something's gotta give!
Red Flags: When Lower Back Pain Becomes Serious
While most lower back pain is annoying rather than dangerous, there are certain warning signs that demand immediate attention. These “red flags” include:
- Severe pain following a fall or accident
- Pain accompanied by fever
- Loss of bladder or bowel control
- Progressive weakness in the legs
- Numbness in the groin or genital area
If you experience any of these symptoms, don't wait – seek medical attention immediately. These could indicate serious conditions like cauda equina syndrome, which requires emergency treatment.
The Pain Scale: Types and Characteristics of Lower Back Pain
Acute vs. Chronic Lower Back Pain
Acute lower back pain is like an uninvited guest that shows up suddenly but usually leaves within a few days to weeks. It's often sharp, intense, and can be triggered by specific movements or activities. Think of it as your back's way of saying, “Hey, something's not right here!”
Chronic lower back pain, on the other hand, is that annoying relative who overstays their welcome. It persists for more than three months and can range from a dull ache to severe, debilitating pain. Chronic pain often develops a mind of its own, becoming less about the original injury and more about changes in the nervous system.
Radiating Pain: When Your Back Pain Travels
Sometimes, lower back pain doesn't stay put. Sciatica, for instance, occurs when the sciatic nerve gets irritated or compressed. This can cause pain to shoot down one or both legs, often accompanied by numbness or tingling. It's like your back is playing a cruel game of telephone with your legs.
Treatment Options: Your Arsenal Against Lower Back Pain
Conservative Approaches
The good news? Most lower back pain responds well to conservative treatment. Rest – but not too much! – is often the first line of defense. Complete bed rest used to be the gold standard, but we now know that gentle movement and activity are usually better for recovery.
Heat and cold therapy can provide significant relief. Ice helps reduce inflammation during the acute phase (first 48-72 hours), while heat can ease muscle tension and improve blood flow. Some people swear by alternating between the two – it's like giving your back a spa treatment!
Physical Therapy and Exercise
Physical therapy is often the MVP of lower back pain treatment. A skilled PT can identify movement patterns that contribute to pain and develop a personalized exercise program. Core strengthening, flexibility exercises, and postural training form the foundation of most PT programs.
Specific exercises that have shown effectiveness include:
- Pelvic tilts – Great for engaging core muscles
- Knee-to-chest stretches – Helps relieve pressure on the lower back
- Cat-cow stretches – Improves spinal mobility
- Planks – Strengthens the entire core
- Bird dogs – Enhances stability and coordination
Medical Interventions
When conservative treatment isn't enough, medical interventions may be necessary. NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen can help reduce inflammation and pain. Muscle relaxants might be prescribed for severe muscle spasms.
For more severe cases, epidural steroid injections can provide temporary relief by reducing inflammation around affected nerves. Surgery is typically reserved for cases where conservative treatment has failed and there's clear evidence of nerve compression or structural problems.
Prevention: Your Best Defense Against Lower Back Pain
Ergonomics and Posture
Prevention truly is better than cure when it comes to lower back pain. Setting up an ergonomic workspace can make a world of difference. Your computer screen should be at eye level, feet flat on the floor, and your back supported by a good chair. If you're stuck with a less-than-ideal setup, even small adjustments can help.
Remember the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds, and take this opportunity to stand and stretch. Your back will thank you!
Exercise and Lifestyle Modifications
Regular exercise is like insurance for your back. A combination of cardiovascular exercise, strength training, and flexibility work creates the perfect storm for back health. Swimming is particularly excellent because it's low-impact while still providing a full-body workout.
Maintaining a healthy weight reduces stress on your lower back. Every extra pound adds approximately four pounds of pressure to your spine. That's some serious math that your back is constantly calculating!
Living with Lower Back Pain: Coping Strategies
Mind-Body Connection
The relationship between mental health and chronic pain is undeniable. Stress, anxiety, and depression can all amplify pain perception. Techniques like meditation, deep breathing, and mindfulness can help break this cycle.
Sleep quality also plays a crucial role. Poor sleep can lower pain tolerance and increase inflammation. Investing in a supportive mattress and maintaining good sleep hygiene can significantly impact your pain levels.
Alternative Therapies
Many people find relief through complementary approaches. Acupuncture, massage therapy, and chiropractic care have all shown promise in managing lower back pain. While the evidence varies, these treatments can be valuable additions to a comprehensive pain management plan.
Frequently Asked Questions
Q: How long does lower back pain typically last? A: Most acute lower back pain resolves within a few days to weeks with proper care. However, chronic pain can persist for months or even years if not properly addressed.
Q: Should I see a doctor for lower back pain? A: You should consult a healthcare provider if pain is severe, persists for more than a few weeks, or is accompanied by red flag symptoms like fever, numbness, or weakness.
Q: Can lower back pain be prevented? A: While not all cases are preventable, maintaining good posture, staying active, strengthening your core, and using proper lifting techniques can significantly reduce your risk.
Q: Is bed rest good for lower back pain? A: Extended bed rest is generally not recommended. Light activity and gentle movement are usually more beneficial for recovery.
Q: When is surgery necessary for lower back pain? A: Surgery is typically considered only when conservative treatments have failed and there's clear evidence of nerve compression or structural problems causing significant functional impairment.
Final Thoughts: Taking Control of Your Back Health
Understanding what lower back pain is – and isn't – empowers you to take control of your back health. Remember, you're not destined to live with chronic pain. With the right combination of knowledge, treatment, and prevention strategies, most people can successfully manage their lower back pain and return to the activities they love.
The journey to a pain-free back isn't always straightforward, but it's definitely possible. Listen to your body, work with healthcare professionals when needed, and don't give up hope. Your back has supported you through countless adventures – now it's time to support it in return.