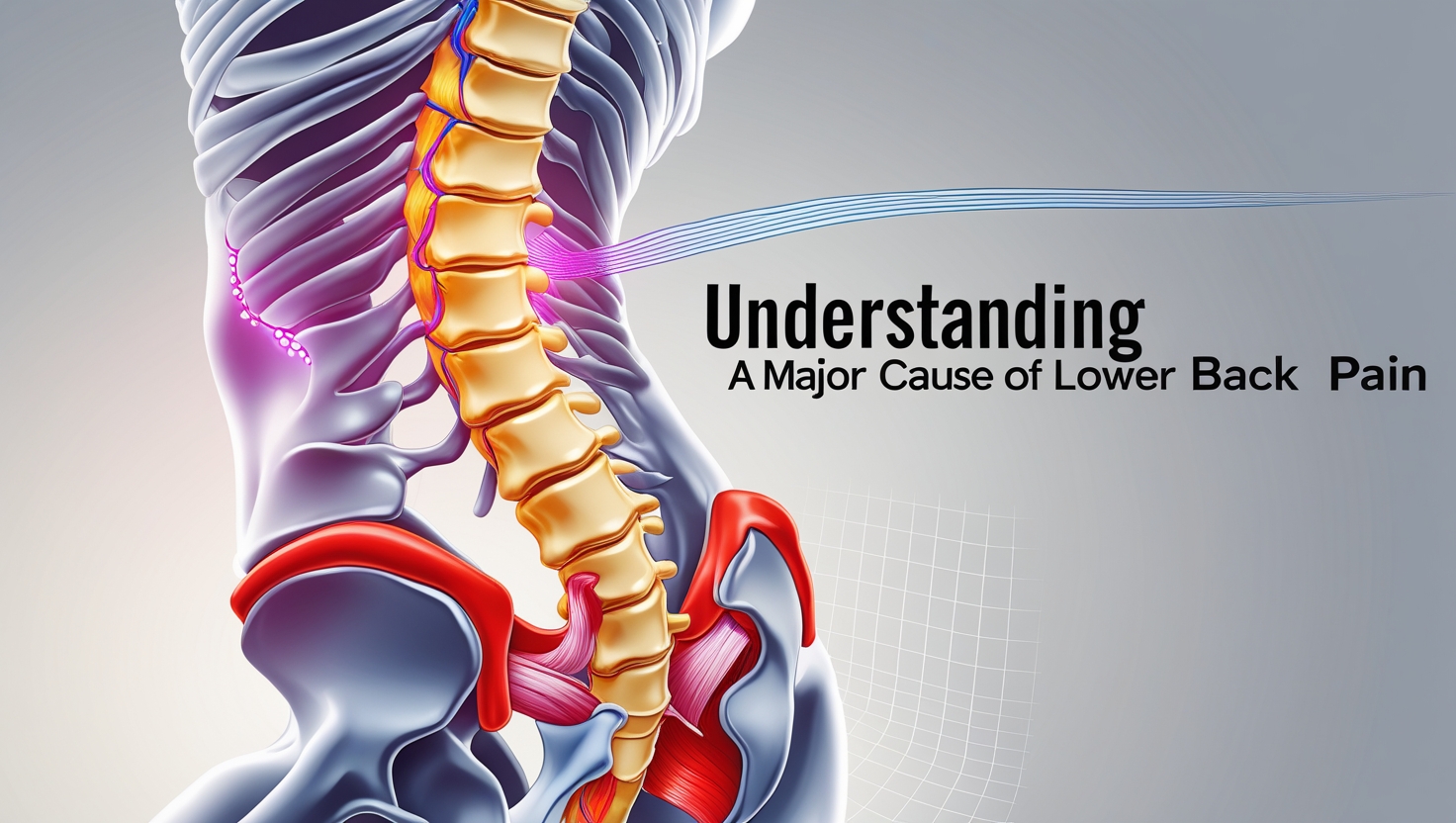
When to Seek Medical Help for Lower Back Pain
Lower back pain affects millions worldwide, but knowing when it's time to see a doctor can be the difference between quick recovery and chronic suffering. This comprehensive guide reveals the critical warning signs that demand immediate medical attention.
Let's face it – back pain is about as welcome as a flat tire on a rainy day. Nearly everyone experiences it at some point, and frankly, most of us just grin and bear it. But here's the thing: while some back pain is just your body's way of saying “slow down,” other times it's screaming “get help NOW!” Understanding when to seek medical help for lower back pain isn't just smart – it's potentially life-saving.
The tricky part? Your back doesn't come with a user manual. One day you're fine, the next you're moving like a rusty robot. So how do you know when that nagging ache needs professional attention versus when you can tough it out with some ibuprofen and Netflix?
Understanding the Red Flags: When Back Pain Becomes an Emergency
Immediate Medical Attention Required
Some symptoms are like fire alarms – you don't ignore them, period. When your lower back pain comes with any of these red flags, it's time to drop everything and seek medical help immediately:
Neurological symptoms top the list of “don't mess around” warning signs. If you're experiencing numbness, tingling, or weakness in your legs, that's your nervous system waving a white flag. According to the American Academy of Orthopaedic Surgeons, these symptoms could indicate nerve compression or damage that requires urgent intervention.
Bowel or bladder dysfunction alongside back pain is what medical professionals call a “cauda equina syndrome” red flag. This rare but serious condition affects the bundle of nerves at the base of your spinal cord. Translation? If you can't control your bathroom functions and your back hurts, get to an ER stat.
Pain That's Different from the Usual Suspects
Not all back pain is created equal, and your body's pretty good at telling you when something's off. Severe, sudden-onset pain that feels like someone hit you with a baseball bat? That's not your garden-variety muscle strain talking.
Progressive weakness in your legs is another game-changer. If you're finding it harder to walk, climb stairs, or even stand up from a chair, your back pain has officially graduated from “annoying” to “needs medical attention.” The North American Spine Society emphasizes that progressive neurological symptoms require prompt evaluation to prevent permanent damage.
The Timeline Factor: When Duration Matters
The 6-Week Rule and Beyond
Here's a reality check: most acute lower back pain improves within 6 weeks. But – and this is a big but – if your pain is still hanging around after this timeframe, it's time to seek medical help for lower back pain. Chronic pain is a different beast entirely, and it requires professional management.
Why 6 weeks? Well, that's typically how long it takes for most soft tissue injuries to heal. If you're still hurting after this period, there might be something more complex going on. Maybe it's a herniated disc, spinal stenosis, or another condition that needs specific treatment.
When “Just a Few Days” Becomes Concerning
Sometimes, though, you don't need to wait 6 weeks. If your pain is interfering with your daily activities – we're talking about struggling to get out of bed, missing work, or avoiding activities you normally enjoy – that's your cue to get help sooner rather than later.
Severity Scales: Rating Your Pain Like a Pro
The 1-10 Scale Reality Check
We've all been asked to rate our pain on a scale of 1 to 10, but let's be honest – it's not always clear what that means. Here's the deal: if your pain consistently sits at 7 or above, and it's not responding to over-the-counter medications, it's time to seek medical help for lower back pain.
Pain that disrupts sleep is particularly concerning. Your body needs rest to heal, and if pain is keeping you awake, you're fighting an uphill battle. Plus, chronic sleep deprivation can actually make pain worse – it's a vicious cycle.
When Pain Changes Character
Pay attention to how your pain behaves. Sharp, shooting pain that travels down your leg (hello, sciatica!) is different from a dull, constant ache. Radiating pain often indicates nerve involvement, which typically requires professional evaluation and treatment.
Age-Related Considerations: When Getting Older Changes the Game
The Over-50 Club
If you're over 50 and experiencing new-onset back pain, the medical community takes it more seriously. Why? Because certain conditions like spinal stenosis, osteoporosis-related fractures, and degenerative disc disease become more common with age.
Osteoporotic fractures are particularly sneaky. They can occur with minimal trauma – sometimes just from coughing or bending over. If you're postmenopausal or have risk factors for osteoporosis, new back pain deserves prompt attention.
Younger Adults: When Age Doesn't Protect You
Don't think being young gives you a free pass, though. Inflammatory conditions like ankylosing spondylitis often show up in younger adults. If you're experiencing morning stiffness that improves with activity, especially if it lasts more than an hour, that's worth investigating.
Associated Symptoms: When Back Pain Brings Friends
Fever and Back Pain: A Dangerous Duo
Fever accompanying back pain is like a bouncer at a club – it's there for a reason, and you should pay attention. This combination can indicate a spinal infection, which is serious business requiring immediate medical attention.
Spinal infections (like osteomyelitis or discitis) are relatively rare but can be devastating if left untreated. They can lead to permanent neurological damage or even life-threatening sepsis.
The Systemic Connection
Sometimes back pain isn't just about your back. Unexplained weight loss, night sweats, or a history of cancer can indicate that your back pain might be related to a more serious underlying condition. These “constitutional symptoms” warrant thorough investigation.
What to Expect: Navigating Your Medical Visit
Preparing for Success
When you do decide to seek medical help, come prepared. Keep a pain diary for a few days before your appointment. Note when the pain is worst, what makes it better or worse, and any associated symptoms. This information is gold for your healthcare provider.
Don't forget to bring a list of all medications you're taking, including over-the-counter drugs and supplements. Some medications can interact with pain treatments, and your doctor needs the full picture.
The Diagnostic Journey
Your doctor will likely start with a thorough history and physical examination. They'll test your reflexes, check your strength, and assess your range of motion. Depending on their findings, they might order imaging studies like X-rays, MRI, or CT scans.
Red flag symptoms will fast-track the diagnostic process. If you're experiencing any of the emergency symptoms mentioned earlier, expect a more urgent workup.
Treatment Options: Beyond “Take Two and Call Me in the Morning”
Conservative Approaches First
Most back pain responds well to conservative treatment. This might include physical therapy, which is often the first-line treatment for mechanical back pain. PT can help strengthen your core, improve flexibility, and teach you proper body mechanics.
Medications play a role too, but they're usually part of a comprehensive approach. NSAIDs, muscle relaxants, and sometimes short courses of oral steroids can help manage pain and inflammation while your body heals.
When Conservative Care Isn't Enough
Sometimes, despite everyone's best efforts, conservative treatment doesn't cut it. That's when interventional procedures might come into play. These can include epidural injections, nerve blocks, or radiofrequency ablation.
Surgery is typically reserved for specific conditions with clear structural problems that haven't responded to other treatments. It's not a decision made lightly, and it's definitely not the first option for most people.
Prevention: The Best Medicine
Building a Strong Foundation
The best time to think about back pain is before you have it. Core strengthening exercises, maintaining good posture, and staying active are your best defenses against future problems.
Ergonomic considerations at work and home can make a huge difference. If you're spending hours hunched over a computer, your back is probably plotting its revenge.
Lifestyle Factors That Matter
Weight management reduces stress on your spine. Every extra pound puts additional pressure on your lower back structures. Smoking cessation is crucial too – nicotine reduces blood flow to spinal structures, impairing healing.
Frequently Asked Questions
Q: How long should I wait before seeing a doctor for back pain? A: If you're experiencing red flag symptoms (numbness, weakness, bowel/bladder problems), seek help immediately. For other types of pain, if it's severe, disrupting your daily activities, or hasn't improved after a few days of conservative care, it's time to get professional help.
Q: Should I go to the ER or my regular doctor? A: Go to the ER if you have red flag symptoms or severe pain that started suddenly. For other situations, start with your primary care doctor or an urgent care center.
Q: Will I need an MRI? A: Not necessarily. Many cases of back pain can be diagnosed and treated without imaging. Your doctor will determine if imaging is needed based on your symptoms and examination findings.
Q: Can I prevent back pain from coming back? A: While you can't prevent all back pain, staying active, maintaining good posture, strengthening your core, and using proper body mechanics can significantly reduce your risk.
Q: Is it normal for back pain to come and go? A: Yes, many people experience episodic back pain. However, if the episodes are becoming more frequent or severe, it's worth discussing with your healthcare provider.
Final Thoughts: Trusting Your Instincts
Listen, at the end of the day, you know your body better than anyone else. If something feels seriously wrong, don't second-guess yourself. Seeking medical help for lower back pain when you're concerned isn't being dramatic – it's being smart.
Remember, early intervention often leads to better outcomes. What might take weeks to resolve if left untreated could potentially be addressed much more quickly with appropriate care. Plus, getting a proper diagnosis gives you peace of mind and a clear path forward.
Your back has to last you a lifetime, so treat it with the respect it deserves. When in doubt, get it checked out. After all, you've only got one spine – might as well take good care of it.